Osseointegration is the result of a biologic response of the bony tissues to implants. For oral endosteal implants a three to six month healing period prior to loading is generally considered a pre-condition for optimal bone apposition to the fixture. This clinical protocol is based on work done by Branemark during the 1960's and 1970's when a final proposition for healing periods for implants of the upper and lower jaw, based on the evaluation of the surgical and periodontal failure rates, was defined (Brånemark et al, 1977 [1] ). These protocols on Osseointegration periods were based on early, partially unfavorable experimental conditions while methods and implant types were continuously changing:
- On edentulous patients with a reduced bone quality and quantity
- With short implant lengths
- With changing less than optimal implant designs
- With changing less than optimal surgical protocols
- With not optimized biomechanically suprastructures
It is therefore not surprising that in the past, the submerged healing period was frequently questioned, based on modifications of surgical and prosthetic procedures. In several animal and human studies the original three to six month healing period was shortened to an early loading protocol. In other modifications, implants were immediately loaded on the day of insertion.

Post-Surgical Bone Reaction
Concerning the bone healing after the surgical implant placement, one can draw the following conclusion:
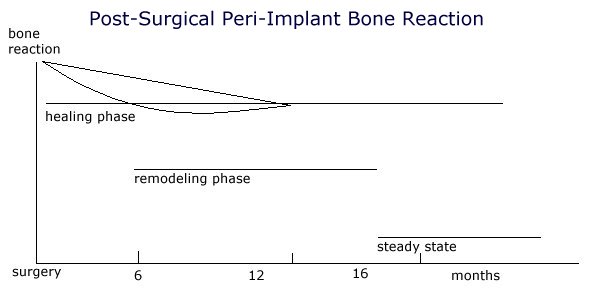
The perimplant bone reaction is initially the highest after the surgical trauma and reduces itself slowly over months, returning to the basic turnover. It is evident that even after the three to six month standard healing protocol any loading will not be placed on the final bony implant bed but bony remodeling will still be in progress.
Based on these two conditions it is not feasible to determine a general healing period depending only on the type of jaw. To define an individual healing period the bone should be evaluated both during and after the implant surgery. Because traditional methods are unsuitable for this measurement, new methods are recently described.
Methods for the evaluation of the peri-implant bone conditions:
Traditional methods Modern methods
Traditional methods Modern methods
The recording of the cutting resistance during the surgery permits some evaluation of the bony structure (compact versus spongious) along the implant site. The measurement of the resonance frequency analysis on an inserted implant provides information about the primary stability between implant and bone. While primary stability in implantology was previously based on a purely subjective evaluation, these two new measurement methods permit an objective recording of the initial implant stability.
Primary and secondary implant stability
To achieve osseointegration an attachment to the bone without any micro-movement is necessary. Prior dental literature cites micromovement of the implant as a causative factor in both the formation of an intermediate layer of connective tissue, which develops between the bone and implant, and osseointegration failure. Initially, primary stability is entirely mechanical. During the healing period however, the biologic processes of osseointegration cause this to change to a mixture of mechanical and biologic stability (secondary stability).
Protocols for immediate or early loading strive for an increase either of primary stability, which can be achieved either through an optimized implant form or implant surface or/and optimized surgical preparation of the implant bed. Conversely, through the modification of the implant surface an acceleration of the bony healing is intended to achieve an earlier osseointegration and therefore a faster acceptable secondary stability (Case examples Fig. 1 - 12).
|
|
|
A 19-year-old patient, with multiple genetically missing teeth, at the end of the preprosthetic orthodontic treatment. In the upper jaw implants are planned in the area 12 - 25. Implants on 12 and 22 should be immediate loaded because of esthetic reasons.
|
|
|
After preparation of the implant bed at the position of both lateral incisors the prospective implant placement will be marked with a direction indicator. Two Brånemark MK IV are inserted and a CeraOne™ abutment is definitively placed on both implants.
|
|
|
Initial implant stability will be measured with the RFA method. The buccal bony defect will be covered using a membrane technique and a prefabricated shell-like temporary will be directly, intraorally rebased over the abutment.
|
|
|
|
Summary
The protocol of successful osseointegration, which was based for over 20 years on the concept of late loading, is increasingly questioned. In several studies successful immediate loading or early loading of implants could be shown. Two indications were described:
- Bar-joint-dentures (Dolder bar) in the lower jaw on 4 - 6 interforaminally placed implants
- Total bridge in the upper or lower jaw on 10 or more implants
The indication for the case selection for immediate loading is based on an optimal stabilization of the implants through a large number (full, horse shoe type bridges) or on implants in a very good bone quality or quantity (interforaminal). Through secondary splinting with the suprastructure, possible micromovement during the healing period can be prevented in both situations.
All protocols up to the present day however show that the operator based case selection on subjective criteria. Objective quantitative criteria for case selection are not yet published. Long term data on immediate, or early implant loading exist only for interforaminally placed fixtures.
At the moment the use of immediate loading still consists of a higher risk because of non-existing, not yet defined diagnostic criteria and can therefore not be recommended to the general practitioner. On the other hand a suitable measurement system will be available in the near future and might revolutionize our treatment concept in implant therapy.














No comments:
Post a Comment